Why It Matters

“If only we’d known that he needed a new pair of shoes.”
This statement came from a care team member in rural Maine about one of her patients. He had come to her primary care office with a complaint about his toes. Upon examination, it was determined that the affected areas would need to be amputated. Eventually, his entire foot had to be removed. But his condition continued to worsen.
It was not until the patient was facing partial amputation of his leg that his care team learned that the patient had a dog. The patient shared how important it was to him to take the dog he loved so much on daily walks. They also learned that he had been going for these walks in an old pair of leaky boots that offered little protection from the snowy, slushy, and wet conditions that are so common in Maine. The patient had been unable to afford more appropriate footwear on a limited income.
Sadly, despite the best efforts of his care team, the patient’s condition continued to deteriorate, and he was no longer able to care for himself at home. He had to move into a care facility without his beloved dog. The care team member who shared this story acknowledged that there were many factors that ultimately contributed to this outcome. She could not help but wonder, however, if things might have turned out differently if the care team had known about this patient’s basic unmet needs sooner.
Jessica Shaffer, the Director of Community Health Partnerships at Northern Light Health in Maine, shared this patient’s story as a participant in the Institute for Healthcare Improvement (IHI)/Pfizer Social Health Learning and Action Network. With funding from Pfizer, IHI created the network to support health care organizations seeking to improve health, well-being, and equity by integrating social health into their health care delivery. Three integrated delivery networks in the US were chosen to participate through a competitive grant award process.
Northern Light Health’s mission is to improve the health of the people and communities that they serve. They submitted a proposal to join the Learning and Action Network to improve the use of social determinants screening and data to recognize and address barriers to health equity in their community. Said Shaffer, “What are we missing by not having conversations about the needs and challenges patients and community members are experiencing? What is important to them and what is preventing them from doing well? Only after understanding these questions can we achieve our mission as a health care system.”
When they first joined the network, the Northern Light Health team determined that three stakeholder groups were crucial to the success of social health integration work and achieving a wide-ranging impact within the system: community partners, clinicians and staff, and patients and families. Each group required an approach tailored to the focus of their work, their priorities, and the intersections of their work. According to Shaffer, “The key to this process is determining how we can better partner or work together to advance some of these needs or some of these impacts.”
As part of the Learning and Action Network, Northern Light benefited from coaching from IHI expert faculty and shared learning from their health system peers. In 12 months, Northern Light made significant progress toward their aim, including:
- Established minimum screening standards for social determinants within their system policy. All patients will be screened at least once every 12 months, and provider teams can choose to screen more often.
- Incorporated a prescriptive analytics platform within their electronic health record (EHR) to identify social risks driving avoidable adverse health outcomes and to provide clinical guidance.
- Sensitized their community engagement team around what will be needed to get more community partners on the platform.
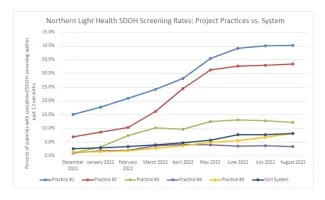
- Social determinants screening across their system increased by 400 percent.
Keys to Success
To make improvements across the entire system, Northern Light Health made key changes that they recommend to others:
- Build community partnerships. The team worked with member hospitals to take inventory of community resources and partnerships. All groups completed an assessment of where and how they currently partner with community-based organizations. In addition, they have completed a gap analysis to identify areas lacking in resources and partnerships needed to advance their health equity work.
- Be clear about the value of collecting data. Data collection can often be an arduous task, especially if it is not clear how the information is being used. During this work, Northern Light Health has developed a better understanding of the usefulness of collecting and analyzing data for improvement. Using data to create reports, dashboards, and other resources have helped them to direct their efforts where they are most needed.
- Engage clinician champions. According to Northern Light Health’s data, champions have been essential. Teams with a practice manager or other staff championing the work reported higher screening rates. Shaffer also shared that one practice had the support of a physician champion who is also chief medical information officer. He sponsored a request to improve the efficiency of screening for social health needs. After the request was reviewed, a recommendation was put forth to incorporate social determinants of health screening reminders into the EHR workflow for clinical staff.
Even with all they have accomplished so far, the Northern Light Health team knows there is always work to be done. With all the valuable data they have collected, they must now decide how to act on the information and who to partner with next.
One focus will be creating community and connection with patients. The Northern Light Health team is working on patient and community communications to raise awareness about why they do social determinants screenings and how the information is being used to serve the community. Northern Light Health will soon launch a community health worker program to help reduce barriers to resources. Though there are always challenges, Northern Light Health is well on its way to better understanding their patients and fulfilling its mission to improve the health of the people and communities they serve.
Elias Miranda is an Institute for Healthcare Improvement Project Manager.
You may also be interested in:
