Summary
- Identifying and standardizing how health care systems and regulators measure violence against health care workers can help predict, prevent, and address such incidents.
The prevalence of workplace violence in health care settings has been steadily increasing, with significant impacts on the safety and well-being of health care workers and the quality of patient care. Health care and social service industries experience higher rates of injury caused by workplace violence and their employees are five times as likely to suffer a violent injury on the job compared to overall workers. A recent survey also found that 40 percent of health care workers experienced a violent incident in the last two years. In addition to causing physical and psychological injury, violence on the job erodes the motivation of health care workers. This compromises the quality of care and puts health care delivery at risk.
This ongoing crisis demands immediate attention and action to ensure a safer work environment. Although violence prevention efforts have become a priority for health care systems, regulators, and policy makers, there is a lack of standardization or best practice recommendations to assist in predicting, preventing, and addressing such incidents.
The Institute for Healthcare Improvement (IHI) Innovation team recently completed a 90-day research cycle to draft a framework that health systems might use to create reliable prediction and response systems to reduce physical violence and improve safety of the health care workforce. We completed a literature scan of existing approaches and frameworks and conducted key informant and expert interviews with approximately thirty experts at 19 health care organizations.
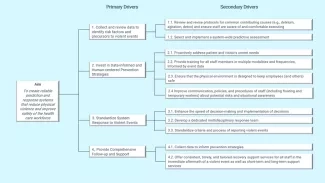
Figure 1 Keeping the Health Care Workforce Safe from Violence Driver Diagram (IHI, 2023)
With these insights, we drafted a driver diagram (Figure 1), highlighted potential changes, and outlined a set of sample measures. We convened an expert panel to validate and revise the existing theory that determined that a key focus should be to develop a common measurement framework for predicting and tracking violence. Using data to reduce workplace violence against health care workers is crucial to provide evidence-based insights to inform corrective actions, mitigate incidents of workplace violence, and accelerate the development of a standardized approach to collaborate across systems.
Pinpointing Issues
While many health care systems have developed internal data metrics and processes to track workplace violence, there is no broader effort to quantitatively understand the problem and identify potential solutions. Robust measurement collection strategies can support a nuanced understanding of the issues within systems and nationally, but this strategy may be complex (in execution and outcomes) and inaccessible for smaller or under-resourced health care systems.
To use data to understand the issue, health care systems must consider their current reporting structure and capacity. First, what data do they currently collect (such as the type of violent event)? Are there identifiable patterns which could help determine pain points? Then, what is the organization’s capacity to manage, analyze, and respond to reported data? Health care systems must have the capacity to act upon the data provided to them. Without a reliable process and follow through, trust in the reporting system may weaken and the quantity and quality of reported data could decline.
Following these considerations, systems should examine a parsimonious set of impactful data points. In a 2023 report, the Massachusetts Health & Hospital Association issued an urgent call for public support to combat the ongoing violence against health care workers. Their survey metrics offered potential measures, including:
- Total number of reported incidents of violence by month
- Aggressors of reported incidents (e.g., patient, visitors, clinician, other)
- Types of reported incidents (e.g., completed physical assault, verbal abuse, threat of harm, attempted physical assault, not contact)
- Victims of reported incidents (e.g., nurse, security officer, aide/tech/other clinician, patient, other non-clinical employee, physician, visitor/companion/other), and
- Reported incident location distribution (e.g., ed, inpatient unit, psychiatric units, outpatient, non-clinical setting, parking lot/campus area, pediatric unit)
A white paper published by Commure, “Safe Healing Environments: Addressing Workplace Violence in Healthcare Through Legislation, Prevention, and Strategic Solutions,” offers further insights into the kinds of metrics to consider when developing a standardized set of measures, including:
- Source of violence (e.g., patient-to-staff, colleagues, patient’s family members, or intruders)
- Patient-related risk factors (e.g., mental health crisis or substance use)
- Environmental risks (e.g., restricted visits, lack of security support, long wait times)
- Staff well-being and patient care quality
Measurement provides data. Data help health care systems and regulators to clearly define issues, develop and test targeted strategies, maintain improvements, raise awareness of the issues, and advocate for public and governmental support.
Next Steps
To bridge the gap, IHI has launched the Keeping Our Workforce Safe from Violence Accelerator Network. Through collaborative efforts and shared expertise, this Accelerator aims to drive meaningful progress towards identifying, creating, and sharing best practice recommendations for workforce violence data measurement, with the goal of preventing and reducing workplace violence in health care settings. The work of the Accelerator is ongoing with plans to disseminate its findings toward the end of 2024.
Other efforts to reduce workplace violence include federal and state legislation, such as the introduction of the Safety from Violence for Healthcare Employees (SAVE) Act in Congress and passage of Texas Senate Bill 240, which requires health care facilities to adopt workplace violence prevention plans by September 2024. Media attention — including a 2023 New York Times opinion piece — helps to humanize the issue.
The strategic use of standardized measurement can enhance efforts to reduce violence against health care workers. Ongoing IHI efforts offer best practices and guidelines on standard measurement to support the prediction and prevention of violent events and assessment of interventions. Effectively addressing workplace violence will reduce physical and psychological injuries, enhance quality of care delivery, restore joy and safety in work, and reduce financial losses.
Kate Feske-Kirby, MA, is an IHI Research Associate.
Photo by ipopba.
You might also be interested in: Centering a More Holistic View of Workforce Safety
