Why It Matters
There is a critical need to redesign our health care system to better serve the needs of older patients. Research has identified specific ways in which the health care system could improve to prioritize these needs. This includes working towards broad goals, such as improved care continuity that has been shown to result in lower hospital utilization for older adults with multiple chronic medical conditions.
It also includes targeted changes that address specific shortcomings. In particular, the 4Ms Framework (Figure 1) offers a set of priorities designed to shift how we think about and provide care for older adults, focusing on four areas: What Matters, Medication, Mentation and Mobility.
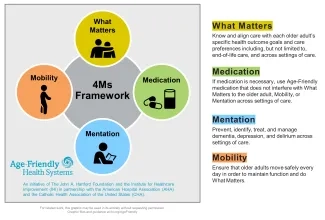
This framework has the potential to transform traditional health care delivery systems into Age-Friendly Health Systems (AFHS) as advanced by a collaboration between The John A. Hartford Foundation and the Institute for Healthcare Improvement (IHI), in partnership with the American Hospital Association and the Catholic Health Association of the US.
The real-world implementation of the 4Ms relies on the ability to adapt the daily work of frontline clinicians as well as engage patients and their caregivers in understanding and managing their health and health care. These activities are driven and reinforced by the IT tools they have available. However, after a decade of significant public and private sector investment in electronic health records (EHRs), there is no national data on how often hospitals are making the investment to use their EHRs to support the 4Ms framework as well as investing in other types of IT to support the unique needs of older adults across settings. For example, EHRs could be adapted to incorporate functions that address the 4Ms by adding prompts and fields in the EHR for clinicians to enter structured documentation of care goals or to review medications known to impact mobility and mentation.
Supported by a grant from the John A. Hartford Foundation, a team of researchers at Harvard School of Public Health and UCSF conducted a national hospital survey to measure adoption of EHR functions that support care for older adults, focusing on structured documentation of the 4Ms (What Matters, Medication, Mentation, and Mobility) and electronic health information exchange/communication with patients, caregivers, and long-term care providers. Results are reported in a new article entitled Hospital Adoption of EHR Functions to Support Age-Friendly Care: Results from A National Survey published in the Journal of the American Medical Informatics Association.
We found that 64.0 percent of hospitals had structured EHR documentation of the 4Ms fully implemented in at least one unit and 41.5 percent had these fully implemented across all units. Structured documentation of medications was the highest (91.3 percent in at least one unit) and structured documentation of mentation was the lowest (70.3 percent in at least one unit). We found that 16.2 percent of facilities had implemented all exchange/communication functions in at least one unit and 7.6 percent of hospitals had implemented across all units. Less than half of hospitals had an EHR portal for long-term care facilities to access hospital information (45.4 percent in at least one unit), sent information electronically to long-term care facilities (44.6 percent), and had training for adults/caregivers on the patient portal (32.1 percent).
Our results offer the first assessment of US hospital implementation of age-friendly EHR functions. Despite the substantial national investment in hospital EHR adoption, implementation has not focused on the specific capabilities to support the care of older adults who comprise the majority of the inpatient population. It is, therefore, unlikely that use of EHRs is resulting in optimal gains in health outcomes for older adults. To address this, it is critical that policy and practice-based efforts, particularly those focused on the care and outcomes for older adults, promote stronger incentives that reward hospitals for such investments.
Julia Adler-Milstein, PhD, is a Professor of Medicine and Director of the University of California, San Francisco Center for Clinical Informatics and Improvement Research.
You may also be interested in:
Learn about becoming an Age-Friendly Health System
Age-Friendly Health Systems: Guide to Electronic Health Record Requirements for Adoption of the 4Ms — An Implementation Guide for Health Systems with Epic Examples
Age-Friendly Health Systems: Guide to Electronic Health Record Requirements for Adoption of the 4Ms — An Implementation Guide for Health Systems with Cerner Examples
