Why It Matters
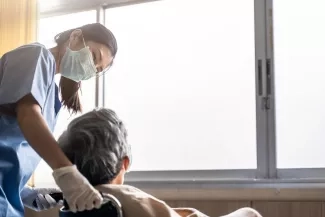
It is sometimes difficult to find bright spots amid the current pandemic, but leading the work of IHI’s COVID-19 Rapid Response Network for Nursing Homes has been a highlight for me. While nurses and doctors working in hospitals have often been lauded as heroes, it has been all too common to underappreciate the efforts of the clinicians and staff caring for often very frail patients in nursing homes.
I am in awe of the over 2,000 people who have registered for access to this Network from across the US. Anywhere from 120 to 150 attendees have been showing up for our 20-minute phone huddles every weekday since June to discuss real-time, pragmatic solutions to problems brought about or exacerbated by COVID-19. In partnership with IHI, these participants have co-created a Nursing Home Driver Diagram & Change Package to reduce COVID-19-related mortality (Figure 1).
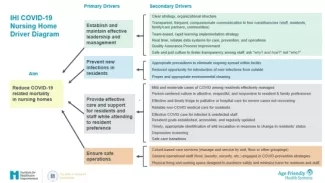
This driver diagram was based on one that originated in South Africa. Using the original as scaffolding, we’ve incorporated content from IHI faculty, input from our Network participants, and other available tools and resources. We could not have created such a thoughtful and robust driver diagram without them.
Nursing homes can use the driver diagram as an assessment tool to evaluate their strengths and opportunities at a high level across four drivers: leadership; infection control; care and support for residents, families, and staff; and patient and workforce safety. Doing this kind of assessment can help nursing homes use the Quality Assurance and Performance Improvement (QAPI) program and Performance Improvement Projects (PIPs) required by CMS to develop a roadmap for addressing COVID-19.
The driver diagram has been co-designed through continuous iterations because what we’re learning about COVID-19 is constantly changing. We designed it to help teams make sense of what can feel like chaos when trying to determine where, of the 150 things that they can do right now, they should focus their attention and in what sequence.
How to Make Meaningful Virtual Connections
Created in partnership with The John A. Hartford Foundation, the goal of the COVID-19 Rapid Response Network for Nursing Homes was to get critical information as quickly as possible to nursing homes struggling with their response to COVID-19. We knew we couldn’t offer something that required too much time for participation, so we designed a daily 20-minute call to address different critical topics each week. Topics included access to personal protective equipment (PPE), lack of testing, hospital-to-nursing home transfers, staff illness and absence, and staff attrition.
Each session has four core components:
- State or federal policy — The COVID-19 policies have been evolving so quickly that participants have appreciated these regular updates;
- Data — This has included updates from epidemiologists on COVID-19 cases and data on what is opening around the country;
- Best practices — We bring in subject matter experts from local nursing homes to spend eight minutes sharing their experience and expertise.
- One good thing — The first thing we do on each call is engage with the community for about two minutes by reserving time and space to think about something positive in our lives. This seemingly small thing helps set a constructive tone for addressing very complicated and stressful problems.
Focusing on “one good thing” might seem trivial or even frivolous given the gravity of the issues we’re addressing. It has, however, been a simple, yet powerful way to build a virtual community and increase joy in work.
We’ve been developing these connections for 16 weeks and I can say, especially after running last week’s huddles, that it’s been meaningful to have this human exchange. People talk about seeing their grandchild for the first time in months. They talk about getting a negative COVID test or the success they’re seeing in their facilities. We really get to see “what matters” to them.
With so many of our ways to connect with people forced online these days, it’s easy to feel disconnected. But this one small practice has helped us get to know one another despite the distance between us. I've been so grateful for these opportunities to connect.
Time for Real Change
In recent months, COVID-19 has highlighted many system inequities in health care that are not new, including in nursing homes. Certified nursing assistants (CNAs), for example, do much of the direct patient care and often know the residents best, but they are typically significantly underpaid. Most do not earn a living wage at a single job and work at multiple facilities to make ends meet. This systemic issue has contributed to the risk of spreading COVID-19 between nursing homes.
The week we spent celebrating and supporting the role of CNAs in nursing home quality improvement was one of my most memorable. It provided an opportunity to talk about the injustice of a system that pays people better to work in a fast food chain than as a nursing home CNA. I’m hopeful that the discussions we’ve started may lead to real change.
Working with the COVID-19 Rapid Response Network for Nursing Homes has renewed and reinforced my appreciation for those working in nursing homes as people and professionals. Over time, many participants talked about their family members in skilled nursing, independent living, or other group living facilities. So, not only are they passionate, dedicated, smart people who want to do the right thing for their patients, they’re also family members of people living in these settings, with a special commitment to continuous improvement.
Jennifer Lenoci-Edwards, RN, MPH, CPPS, is Head of the North America Region, Institute for Healthcare Improvement.
You may also be interested in:
How to Talk About COVID-19 and Your Patients Wishes Regarding Serious Illness Care