Why It Matters

Photo by Gary Bendig | Unsplash
Setting measurable targets is a classical management practice to boost operational performance. In some cases, this approach has led to results, but targets have also led to unintended consequences. At the National Health Services (NHS), a target that places a ceiling on the amount of time patients can spend in the emergency department has been widely evaluated and critiqued. In reviewing the use of targets, the Health Foundation concludes: “Targets are one means to achieve progress against a priority, but not all priorities lend themselves to a target.”

Figure 1. The percentage of admitted and discharged patients who left the department at time periods from arrival. On the Y axis is the percentage of patients; on the X axis is time (in minutes) in the emergency department.
The data displayed above for most hospitals follow a similar pattern — as the 4-hour target approaches, many patients are admitted to the hospital, with a slight bump in those discharged, as providers hurry to meet the target. As a result, the target leads clinicians to move patients through the system at the last possible minute, potentially resulting in unnecessary admissions. In some cases, it may even decrease the urgency with which patients are admitted or discharged, since it conveys to providers that any time in the ED under four hours is acceptable.
Targets set by management can help indicate the magnitude of change required, but they’re often over-used. In fact, W. E. Deming, the management thinker who helped found the field of quality improvement, calls out targets as problematic in one of his renowned 14 points for management. Point No. 11 is to “eliminate slogans, exhortations, and targets for the work force asking for zero defects and new levels of productivity.”
Why? Targets that mandate performance beyond the capability of the system can lead to distortion like we see in the ED example. In The New Economics, Deming described three ways to meet a target without system improvement:
- Redefine the terms — In the ED example, this could involve admitting patients to hallway spaces instead of designated unit beds.
- Distortion and faking — In patient flow, this could involve submitting inaccurate data.
- Run up costs — For example, units could add unnecessary beds, staff, or other resources.
In a culture where accountability is a key management strategy, staff will often resort to one of these approaches to meet a target.
The study of complex systems provides a framework for understanding why targets may not be the best strategy for driving improvement. Hospital-wide patient flow is an example of a complex system with interconnected parts and processes: the emergency department can only admit patients if beds are available in other units, so delayed discharges from those units have a huge impact on emergency department wait times, to provide just one example.
Learn More: IHI Hospital Flow Professional Development Program
To improve hospital flow without distortion, leaders must look at the whole system of care processes, not just performance within individual patient care units or for subgroups of patients. Systems thinking requires viewing the organization as dynamic: adaptive to the needs of patients, and comprised of interdependent clinicians and staff, departments, patient care units, infrastructure, and processes all working toward a common purpose. Optimization of a system requires orchestrating the efforts of all components of the system toward achieving hospital-wide patient flow.
In conjunction with quality improvement strategies, the adoption of a few “simple rules” can catalyze a systems view to guide decision making and action. Research on complex systems has found that simple rules can to lead to high levels of performance of a system. The behavior of a flock of birds in flight is an example of this phenomenon.
Flocking behavior is controlled by three simple rules:
- Separation — Avoid crowding neighbors.
- Alignment — Steer toward average heading of neighbors.
- Cohesion — Steer toward average position of neighbors.
With these three simple rules, the flock moves in a harmonious way, creating complex motion and interaction that would be extremely hard to achieve otherwise.
Can we find simple rules like these to optimize hospital-wide patient flow? Such rules should provide guidance and a vision for clinicians and staff, but they should not be prescriptive solutions. We propose the adoption of these three simple rules for achieving hospital-wide patient flow:
- Right Care, Right Place — Patients are placed on the appropriate clinical unit alongside the clinical team with disease- or condition-specific expertise.
- Right Time — There should be no delay greater than two hours in patient progression from one hospital unit or clinical area to another, based on clinical readiness criteria. For example, patients should be transferred within two hours from the ED to an inpatient unit, within one hour from a PACU to a surgical unit, and discharge to home or community care within two hours.
- Operational Capacity — Teams should ensure each unit or clinical area has operational capacity at the beginning of each day. For example, a unit should have one or two beds available and staffed at 7:00 AM based on patient demand patterns.
These simple rules are not intended for judgement or accountability. Rather, they can form the basis for a hospital-wide flow philosophy that unites all staff and departments to a common purpose. They can provide the basis for daily flow huddles to manage safe and timely patient progression throughout the hospital.
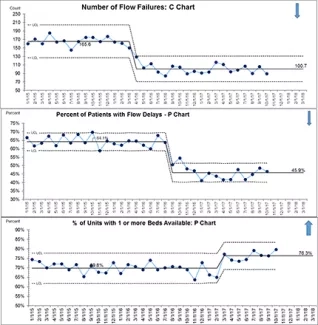
Most importantly, they can form the basis for learning and improvement through quality improvement methodologies. Measuring each rule provides data for learning about the flow issues throughout the hospital. The executive leadership team, who is ultimately accountable for achieving hospital-wide patient flow, can create a hospital-wide learning system to understand failures to achieve these simple rules and focus improvement efforts on mitigating the failures, including through run charts and control charts, such as the ones below.
Managing hospital operations to comply with targets often leads to workarounds and other distortions of the system. Instead, adopting simple rules and a system-wide learning system can be a more effective strategy for complex systems to achieve hospital-wide patient flow.
Lloyd P. Provost is Statistician and Senior Improvement Advisor at Associates in Process Improvement. Patricia Rutherford, RN, MS, is a Vice President at the Institute for Healthcare Improvement.
You may also be interested in:
IHI white paper – Achieving Hospital-wide Patient Flow
