Why It Matters

What does it mean to be age-friendly? At its most basic, it means providing safe, high-quality care that lines up with what matters most to an older adult. In the following interview, Mary Tinetti, MD, Chief of Geriatrics at Yale School of Medicine and Yale-New Haven Hospital, and co-chair of the advisory group for IHI’s Age-Friendly Health Systems initiative, explains the keys to providing the best care possible for older adults.
What defines an age-friendly health system?
In an age-friendly health system, all the people who work in the health system and interact with patients are familiar and comfortable with, understand, and are competent at addressing what matters to each individual. They know how to adjust their interactions to meet each person’s needs. This is whether they clean rooms or welcome patients into an office or they’re clinicians, social workers, or physical therapists.
To do that, you must understand that people accumulate more conditions and become more complex as they age. They may have some vision and hearing difficulties that need to be recognized and adjusted for. They may have mobility issues, so they need more help moving around. Most importantly, we must recognize that older individuals vary in what matters most to them. Some of them want their blood pressure as tidy as it can be or their glucose perfect, spot-on. Others are more concerned with feeling comfortable and not burdened by their health care from day to day. Faced with tradeoffs across many conditions and treatments, older adults vary in the outcomes they most value and desire. Being age-friendly means recognizing and responding to individuals’ different needs, interests, and priorities.
What do some clinicians misunderstand about providing care to older adults?
Most clinicians try to do their very best to provide good care to their older adult patients. The problem is, as clinicians, we learn how to treat diseases. That works fine if you’re 21 or 45 or even 80 and have one disease. The problem is, as we age, we often accumulate, and must manage, not only more diseases and conditions, but also more life issues, such as losing a spouse, financial insecurity, or sensory, physical, or memory limitations. These changes all complicate our ability to take care of each one of those conditions and decrease the likelihood that each treatment will help the outcomes that matter most to the individual.
Well-meaning specialists may try to treat one disease and make two or three other diseases worse. Or they may not focus on the outcomes that matter most to the patient. You need to have a broader vision when there are multiple things happening in a patient’s life.
Sometimes it’s unfamiliarity or uncertainty on the part of clinicians. They don’t know what to do with all that other information [about a patient’s life or health], so it's easier to focus on what they do know. Unfortunately, though, there may be unintended consequences as a result of ignoring all that life context and complexity.
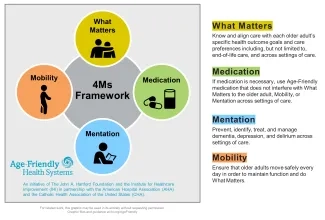
A central part of the age-friendly approach is focusing on improving care on the so-called “4Ms.” How do you explain this focus and why it’s important?
By creating the 4Ms, we’re trying to make care that is very complex more manageable. We’ve identified the core issues that should drive all care and decision making for older adults. The 4Ms apply regardless of your individual diseases because these are the areas that are affected by essentially all diseases. They also apply regardless of how many functional problems you may have, or your cultural, ethnic or religious background.
The 4Ms are:
- What Matters — This means acknowledging that older adults vary in what matters most to them about their health and their health care;
- Medication;
- Mentation — This includes the “three Ds” of the 4Ms (depression, dementia, and delirium); and
- Mobility.
These are the four areas that emerged as being the core of care when we looked at the last 40 to 50 years of research into the care of older adults. If they work well, they are the things that help you live your life. If they don’t work well, they keep you from doing what you want in life.
Why is it important for health care providers to approach the 4Ms as a set of interventions rather than individually?
Two key reasons: 1) If you focus on one problem when there are multiple things happening, you may make that problem better, but you may make three other problems worse; and 2) it simplifies the care and the management of older adults because these 4Ms are intricately related to each other.
For example, the medications you need to target to provide age-friendly care — like opioids or sedatives, for example — are those that can not only cause a lot of adverse effects, but they can also impede mobility and thinking. They can also lead to confusion in the hospital, more depression, and can impede the ability to do what matters most to a patient, like staying alert or communicating clearly with their family members.
Simplification is key because — if age-friendly health systems had to deal with each of the 4Ms independently — there might be 20 things to do. We were able to pare it down to about five things because what helps thinking and memory usually also helps mobility. And taken together, what helps memory, thinking, and mobility, helps people do what matters most to them. In other words, you simplify what you have to do and multiply your positive outcomes by addressing all of the 4Ms as an entity.
How might the age-friendly approach work in a patient’s life?
A patient with Parkinson’s disease can help us understand why using the 4Ms is important. Parkinson’s disease affects walking and other movement, but it also affects parts of the brain that help with memory, problem-solving, and carrying out tasks of daily life.
There are medications for treating Parkinson’s that will help with mobility, but they can make thinking worse. So, if a clinician just focused on improving somebody’s mobility, your treatment plan could contribute to confusion or memory difficulties. On the other hand, if you ignore treating someone’s mobility, they may not be able to do what’s important to them.
This is where the what matters communication comes in. “From what you’ve said, Mrs. Smith, I understand that what matters most to you is to be able to walk to the corner store and pick up your groceries twice a week.” To do that, she needs to be able to walk. She also needs to remember what she wants to get at the store and how to find her way back home. If you just say, “I see your tremor is worse. Let’s increase your Sinemet,” and Mrs. Smith gets more confused, she can’t do something that’s important to her. On the other hand, if we say, “This medicine is making you too confused. I think we need to stop it,” and then she can’t move, then she still can’t do what matters to her.
The age-friendly approach means saying something like, “Mrs. Smith, I recognize it’s important to you to be able to walk to the store and get your groceries. Let’s look at your medications. Let’s balance them to get the right amount of Sinemet. Let’s stop this other medication that may be making you a little confused, and then let’s see if you’re able to maintain your mobility without making your memory worse.”
With older adults, there’s always a tradeoff. All the tradeoffs are why it simplifies care planning to ask what matters most to the patient because it helps you determine where to focus. If you put what matters most to a patient at the center of decision-making discussions, then you can balance everything else. Identify the activities that matter most to them, and then modify the medications.
Are any of the 4Ms more challenging than others for a lot of organizations?
Identifying and supporting what matters most for patients is often challenging. It’s difficult for a lot of reasons. Number one is our health care system is not a health care system. It’s a disease system. From the foundations of how clinics and hospitals are set up, to how clinicians are trained, it’s all about the diseases.
Number two is that many of us were not trained to discuss what matters. There are some exceptions, of course. Nurses, social workers, and therapists, for example, are often trained to identify what matters most to patients, but many physicians aren’t. It can seem overwhelming to us because what we need to do feels outside of our expertise. “I became an orthopedist because I like to do joint replacements. Whether or not somebody wants to go to a senior center is not something I’m comfortable discussing.” So, a lot of the difficulty is the discomfort, lack of competence, and questions we don’t know how to answer.
Fortunately, a lot of evidence has emerged in the last 10 years that suggests that all of us can learn to talk about what matters most to patients, regardless of our specialty. We’re not asking orthopedists to become social workers, but how can your expertise — no matter what that expertise might be — lend itself to helping an individual identify what matters most to them? For example, when you’re talking with a patient trying to decide whether they need a joint replacement, the conversation is not just about what their x-ray looks like, or even how much pain they’re having. The discussion is about whether the surgery will let them do more of what matters most to them.
Why is providing age-friendly care personally important to you?
My mother had many chronic conditions and often got conflicting information as she went from clinician to clinician. The last time I went to see her before she went on home hospice, she was in the hospital and couldn’t breathe and said, “I never want to come back again.” I saw her having accumulated multiple conditions and getting a lot of health care, but not necessarily what mattered most to her. In contrast, I have a 96-year-old father who I am happy to tell you takes only two medications. He doesn’t need all that much from the health care system. So, I’ve seen up close the different trajectories people can have. As a geriatrician, I see it every day.
I see the wonderful things that our health care systems can do, but I also see the unintentional harm we can do. And I don’t just mean the obvious things like operating on the wrong side or infections that should be avoided. I’m talking about the unintended consequences of what many people consider good health care. That’s what drove me to think, “I have to try to do something about this.” It is very personal when I see the effects of health care on a lot of people, and I know it can be better.
Editor’s note: This interview has been edited for length and clarity.
Age-Friendly Health Systems is an initiative of The John A. Hartford Foundation and the Institute for Healthcare Improvement (IHI) in partnership with the American Hospital Association (AHA) and the Catholic Health Association of the United States (CHA).
You may also be interested in:
