Why It Matters
Three months before the pandemic first surged in the US, Gregg S. Meyer, MD, MSc, helped announce that Mass General Brigham (Boston, Massachusetts) was launching a massive digital health initiative. Much of what was expected to take years happened almost overnight because of COVID-19 protocols. Now President of the Community Division and Executive Vice President of Value-Based Care for Mass General Brigham, Meyer describes in the following interview the complexities and possibilities of providing virtual care. He was one of the co-chairs of the IHI Lucian Leape Institute expert panel that contributed to the IHI Telemedicine: Ensuring Safe, Equitable, Person-Centered Virtual Care white paper.
How can health care prioritize patient safety in telemedicine?
The key is to ask some important questions: How can we use telehealth, telemedicine, and digital care as tools to address safety gaps? What are the potential gaps being created by using these tools to deliver care? What are the risks of delivering care remotely?
In safety science, you want to have a balanced view of both benefits and risks. Telehealth can be used to fix gaps in safety — for example, the ability to actually see what medications patients are taking by asking them to use their smartphone or tablet to show us what’s in their medicine cabinet. At the same time, we need to identify when virtual care is most appropriate and when we need to be face to face, and it’s important to consider issues that might be introduced when communicating virtually.
Your organization, Mass General Brigham, launched a major digital health initiative at the end of 2019. How has the COVID-19 pandemic influenced the telemedicine part of this initiative?
We started the initiative after looking at how other sectors of the economy are fundamentally changing how they interact with individuals and other organizations by using technology — most interactions are digital. Technology enablement came together at the same time with consumer demand. For example, consumers these days expect to be able to bank or buy groceries online. Our organization recognized that digital enablement was what people also want and expect in health care, and the tools have gotten good enough to support more virtual capabilities. Mass General Brigham had also made a major investment in an enterprise electronic health record and recognized that virtual care is one way to get more value from that technology.
So, we developed a cogent, well-paced plan to roll out virtual care over a period of two to three years, beginning in 2019. Prior to the pandemic, 0.2 percent of all visits were virtual. The pandemic hit and within six weeks, 62 percent of all visits were being done virtually. We scaled up at lightning speed. In fact, in a period of six weeks we accomplished more than we had hoped to accomplish in three years.
I think two key things enabled this. First, the overwhelming need spurred by the pandemic removed many of the barriers and politics involved in implementing virtual care because people couldn't come into the hospital and we were essentially shut down to outpatients, yet we had to meet the need. That created a climate of moving very quickly. Second, it was essential that our health system already had this plan underway to implement more virtual care. We had made the initial foundational investments in virtual care so that we could move very quickly and, not surprisingly, it stuck. Even when people could come back to the hospital, the proportion of virtual visits decreased but not to pre-pandemic levels. Virtual visits are currently hovering somewhere between 20 percent and 30 percent, higher in some areas like psychiatry — where many patients like virtual care even better than face to face — and not as high in other areas where care may not be so easy to deliver virtually (e.g., in instances when physical exams are necessary). The pandemic is an incredible accelerant of virtual care, particularly for organizations that already made foundational investments, and made it very clear that we’re not going back to where we used to be.
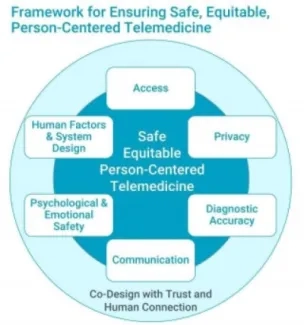
Figure 1. Framework for Ensuring Safe, Equitable, Person-Centered Telemedicine
Psychological and emotional safety is one of the six elements of the IHI Framework for Ensuring Safe, Equitable, Person-Centered Telemedicine (Figure 1). What practices or behaviors can help organizations and practitioners address psychological and emotional safety in telemedicine?
In the past, we delivered care to inpatients, in an outpatient ambulatory setting, or maybe even in the home setting. Now there is a whole new way of delivering care — inpatient care, outpatient care, and virtual care. We have a lot of learning to do to provide virtual care that is safe and ensures a good experience. For example, being cognizant of things like you are being invited into somebody's home via the technology. That is a great learning opportunity, but it's also a little invasive. You need to be aware of those things and understand the limitations and what you might lose with a virtual visit.
One advantage is that patients say clinicians generally have more eye contact in a virtual visit because during an in-person visit we’re often turning away to look at the computer. A disadvantage of a virtual visit, however, is not being able to see the patient’s body language as well. Making virtual care feel safe entails being mindful that the patient is giving you a window into their life, and you need to make sure the patient is comfortable with this. Clinicians may also need to explain things a little bit differently when using virtual care. For example, you can’t demonstrate something quite as clear as you can in person. You may also need to more frequently check that the patient heard things consistently and they really understand your language.
One way to ensure psychological safety is for both patients and providers to agree on what we can accomplish together, in this virtual interaction, and also what we're going to give up. Both need to treat each other respectfully and patients need to be able to say when they’re not comfortable — for instance, being able to turn off their video or being explicitly asked by the clinician if the visit can be recorded, if needed. That's a discussion that clinicians need to have with patients. The concept of what “webside manner” entails is important, especially being kind and thoughtful about where someone else is coming from, and doing that in a digital world requires attention.
Another advantage of virtual visits is that they make it easier to include a patient’s —particularly an elderly patient’s — children or other loved ones in the visit and conversations about their care. It’s very disruptive for a loved one to arrange to come to an in-person visit. But virtual care makes it easier to include someone who might be half a country away. That is incredibly powerful.
On the other hand, many of the advantages of virtual care have downsides that need to be carefully considered such as patient privacy, communication style, and recording virtual visits. Recording, for example, makes it easier for patients to remember the details of what they need to do next and to have access to the recording after the visit for themselves and perhaps to share with a family member. That can be very helpful, as long as it’s done with permission. The flipside of this advantage is protecting patient comfort and privacy.
What excites you about the future of telemedicine?
One significant gain of using virtual visits is that clinicians can better understand a patient’s context. I've had patients who've essentially given me a tour of their personal space, and I can ask them, “What’s in the refrigerator? What’s in the medicine cabinet?” We’re now essentially doing virtual house calls efficiently and at scale. Another exciting aspect is that virtual care presents another way to encourage co-production and patient participation in their care.
What assumptions about telemedicine need to be challenged?
We often underestimate people’s ability to interact digitally and often assume that people of a certain age may be less comfortable with using technology. In my experience working in a health system and as a primary care physician, I was skeptical about how useful some digital tools would be or if patients would use the portal to interact with us asynchronously. That concern was unfounded. I found that when we asked patients, many of whom were elderly and had limited access to broadband, to fill out a survey before their visit, many came in for their visits and had these surveys completed. I asked one patient how he did it. He replied that he didn’t have internet access, but the town library does, and three or four days before his appointment, he’d go to the library to complete the survey. If he needed help, the librarians or someone else at the library or sometimes his grandchildren would provide help.
We also sometimes underestimate what we can do virtually to examine people. I can do a formal test in an office that I can’t reproduce exactly in somebody’s home, but I can have them walk up a flight of stairs with their phone in hand to hear whether they’re short of breath. I can watch them walk across the room and navigate their house. I can have them do some relatively simple maneuvers and be able to understand a little bit better what’s going on.
What are some of the telemedicine equity issues that health care needs to address?
We always have to think about people who don't have access to smart screens. How are we going to care for them? Sometimes that means using the old-fashioned telephone. We also need to advocate for broadband access. Broadband should be as much a human right as having running water and electricity.
Editor’s note: This interview has been edited for length and clarity.
You may also be interested in:
Telemedicine: Ensuring Safe, Equitable, Person-Centered Virtual Care white paper
