Summary
- “The power of seeing someone on their turf, with the things they love, and the people they love, is so valuable, and makes [clinical] care more effective,” said Shivani Jindal, MD, MPH.
Sometimes clinicians jump to unhelpful conclusions when they label a patient as “noncompliant.” According to Shivani Jindal, MD, MPH, “Rushing to judgement is a mistake.”
Jindal is an Associate Professor at the University of Cincinnati College of Medicine and Director of Transition of Care for the Cincinnati VA, a health care provider for US war veterans and retired military personnel. The US Veterans Health Administration (VHA) is part of Age-Friendly Health Systems (AFHS), an initiative of The John A. Hartford Foundation and the Institute for Healthcare Improvement (IHI), in partnership with the American Hospital Association (AHA) and the Catholic Health Association of the United States (CHA).
In a recent interview with IHI, Jindal recalled the case of one of her home care teams’ patients. He was part of the Hospital in Home program that provides acute in familiar home surroundings.
The patient was a veteran with heart failure who was not taking his prescribed diuretic every morning. Instead of making assumptions about her patient’s choices, Jindal took the time to establish a relationship.
One side effect of the medication was frequent urination. During her home visits, Jindal learned that this meant the patient did not feel comfortable going out for after taking it. This may not at first sound like a critical issue. However, the patient eventually shared why it mattered so much to him.
“It turned out that this gentleman really liked going to have a morning coffee with his Veteran buddies,” Jindal explained. The treatment she had prescribed had inadvertently forced him to choose between spending time with his friends and staying on his medication as prescribed.
This revelation led to Jindal and her patient co-designing a solution. They talked about how he could identify a window of time to take his medication that worked with his schedule for the day. The patient was then able to maintain the relationships that meant so much to him and take the medications he needed to avoid hospitalization. Without learning more context, Jindal could easily have assumed the worst about her patient’s willingness or ability to follow his care plan. “Being in a patient’s home helps us to see the whole picture and exercise shared decision making,” Jindal stated.
No Place Like Home
Before specializing in home care, Jindal was an inpatient hospitalist and then worked in post-acute care in a nursing home. Her introduction to home care during a geriatrics fellowship proved to be a transformative experience. “The power of seeing someone on their turf, with the things they love, and the people they love, is so valuable, and makes [clinical] care more effective,” she said.
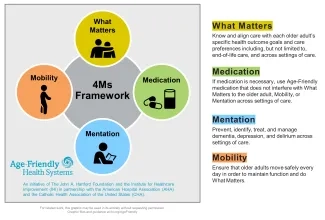
Figure 1. 4Ms Framework of an Age-Friendly Health System
Jindal expressed appreciation for how the Age-Friendly Health System 4Ms Framework provides a structure for thinking about home care for older adults. “I think Age-Friendly Health Systems . . . is an effective tool to help with those gaps in the continuum of care,” she stated, “and it covers some common geriatric syndromes we all see.” In Jindal’s experience, 4Ms-focused care is especially important when providing care to Veterans who may have had negative experiences with health care in the past. She shared the following observations about how using the 4Ms Framework has helped her care for Veterans in their home settings:
- What Matters — Sometimes asking about What Matters can have a profound effect on the clinical interaction. Jindal’s team has heard many Veterans say, “Wow, no one has asked me what matters before,” she reported. They say they have never had a clinical team ask about their values or ask what they do and do not like about their care. Jindal noted the importance of giving patients the opportunity to guide their care but also to avoid misunderstandings. “Sometimes a caregiver, clinician, or family member may be doing something for an older adult [because they think it makes] them happy,” Jindal explained, “but what actually matters to them [may be] something else.” She continued, “It is important to peel back those layers and have that conversation. It can completely change the care you are giving.”
- Medication — Jindal noted that providing age-friendly care means conducting a meaningful medication assessment that does more than ask a patient whether they are taking their medications and how. It means understanding what medications poses high risks when prescribed for older adults. It also means taking the time to explain medication issues to the patient or their caregiver. Jindal adds that providing care in the home setting offers opportunities to understand a fuller picture of a patient's life. This could include, for example, problems affording to fill prescriptions or an undiagnosed cognitive condition causing confusion or forgetfulness.
- Mobility — Jindal appreciates that, when providing age-friendly care, addressing mobility means more than focusing on injuries from falls. “[Clinical] training teaches us always to think about falls, but [with age-friendly care] we focus on tying mobility function back to the goal: What Matters. Is there something the patient wants to be physically able to do?” she explained. Understanding this can help tap into a patient’s intrinsic motivation to work on mobility.
- Mentation — Jindal notes that the Age-Friendly Health Systems approach to mentation — addressing dementia, depression, and delirium — helps to remove some of the stigma around mental health and older people. “There is a lot of ageism out there,” Jindal asserted, “an assumption that ‘depression is normal when you’re older,’ for example, which is not true.”
Beyond specific areas of clinical care, Jindal described how she uses the 4Ms as an organizing framework, including to set the agenda for her team’s daily huddle. “I even formulate my notes with [the 4Ms] framework,” she shared.
Jindal also uses the 4Ms for educational purposes. “I think [the 4Ms] framework is such a wonderful teaching [tool],” she said. “I use it to teach med students, residents, and our interprofessional trainees. I use it to teach colleagues. We’re using it as part of the fabric of our programs.”
Age-Friendly Home Care: Benefits for Patients and Clinicians
In Jindal’s experience, providing age-friendly home care helps connect her to the human aspects of her work that she finds most meaningful. “Not everyone is going to bare their soul to tell you everything that is bothering them because that can be hard to do,” she explained, “but we see what responsibilities that person has, what other burdens they may be carrying.” Over time, Jindal has learned to be observant. “You gain a lot of nonverbal information just by looking around when you’re sitting there at the dining table or on the couch. There is dignity and pride there.”
Patients also benefit from age-friendly home care because many older adults would rather receive high-quality care in the comfort of their own home. “I think a hospital without walls is what people want,” Jindal stated. “Over 90 percent of older adults want to age at home. They don’t want to go to a facility.”
Given how much home health care can vary from agency to agency and state to state, Jindal highlighted the value of using the “shared language” of the 4Ms to help standardize high-quality home care delivery and support better continuity of care. In partnership with the Hartford Foundation, the AHA, and the CHA, IHI is working through its Age-Friendly Health Systems initiative with home health care providers across the United States to develop a 4Ms implementation guide for Age-Friendly Home Health Care.
Explore ways to get involved and join the Age-Friendly Health Systems movement
Using the 4Ms Framework, and guided by What Matters most to a patient, clinicians and patients can identify gaps in care and support to co-design realistic goals and plans.
“If you’re thinking about implementing the 4Ms Framework or something like it, you have to have a team-based approach to care, and it has to include the patient,” Jindal advised.
Charlie Goodwin-Smith is an Institute for Healthcare Improvement Project Manager.
The views expressed in this post belong to Shivani Jindal, MD, MPH, and not the University of Cincinnati College of Medicine, the Cincinnati VA, or the US Veterans Health Administration.
Photo by Peter Burdon | Unsplash
You may also be interested in:
To help understand what matters most to patients, share this new guide, My Health Checklist, with them in advance of each home health visit.
