Why It Matters

Photo by Afif Kusuma | Unsplash
The following is an excerpt from the Telemedicine: Ensuring Safe, Equitable, Person-Centered Virtual Care white paper.
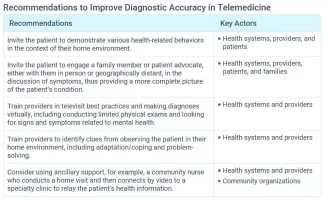
Telemedicine presents new challenges for diagnosis. Providers must learn how to address and overcome these risks when possible and determine when a virtual visit is not appropriate because the risk of diagnostic error is too high.
Diagnostic errors are one of the most prevalent safety issues in ambulatory care and this risk can be exacerbated by a virtual visit. In one study, more than 40 percent of respondents expressed concern about their ability to get a proper treatment or diagnosis virtually. During an in-person interaction, a provider can observe a more complete presentation of the individual before them. For example, a skin rash can be viewed from more angles and the provider can touch the area of concern for a more complete assessment of the issue.
Moreover, clinicians often rely on other forms of observation to fully assess a patient’s condition. Observing body language, personal behaviors, and other individual characteristics can offer a more complete picture and reveal opportunities for intervention. In addition, telemedicine visits typically involve an interaction between a single provider and the patient, while office visits often involve interactions with other care professionals, including nurses, medical assistants, and technicians, all of whom can inform the final diagnosis.
That said, telemedicine also has certain advantages. Video-enabled visits offer the opportunity to see the patient in context, and therefore providers may observe their living situation and how they interact within their environment. For example, the provider might ask a patient to go to the refrigerator and open a bottle or can, which enables the provider to observe the patient’s mobility and dexterity as other inputs to inform diagnosis. (Of course, if the patient prefers greater privacy, as discussed above, their wishes must be respected.) Another benefit of televisits is that the technology makes it possible to engage family members or others who may be geographically dispersed, but able to contribute a valuable perspective. Finally, because a patient typically interacts with only one provider during a televisit, this type of visit may provide valuable additional time for uninterrupted conversations between patient and provider that help improve communication and inform diagnosis.
Another diagnostic risk associated with telemedicine is overreliance on technology. Over the last 20 years, health care systems have recognized that diagnostic errors often occur when physicians rely on the electronic health record (EHR) or other technology to alert them if something is wrong. In a televisit, there is less opportunity to directly observe and examine the patient, and thus providers may be more inclined to rely on patient charts and records. With a relatively limited physical exam possible during a virtual visit, the provider may be too dependent on patient history and laboratory findings to inform a diagnosis. Providers must be keenly attentive to ensure that they thoroughly check and review information with patients during televisits, and that they can distinguish when an in-person visit is truly needed.
Diagnostic Accuracy is one of the six elements of the framework for ensuring safe, equitable, person-centered telemedicine. To learn more, download the free Telemedicine: Ensuring Safe, Equitable, Person-Centered Virtual Care white paper.
You may also be interested in:
Telemedicine: Co-Designing Care for the Future, Not Just for the Pandemic
