Summary
- Through a collaborative effort, the care team at a Community Living Center identified changes to improve an older adult’s health based on what was most important to her. “The heart of geriatrics is interdisciplinary,” said Dr. Priscilla Yee.
Carmen (not her real name; some details have been changed) had a tough time when she returned to the long-term care facility where she lived. After a hospitalization, she was no longer able to mobilize as she had before her illness. She was frequently upset, with uncontrollable crying spells. She was diagnosed with depression, other mental health conditions, and failure to thrive because of her increasing frailty and overall decline.
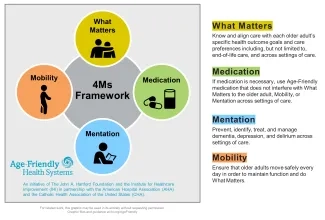
Earlier in the year, the Community Living Center (CLC) at the Hampton VA Medical Center (Hampton, Virginia, USA) earned recognition as an Age-Friendly Health Systems Participant. Participant (or Level 1) teams have successfully developed plans to reliably implement a set of evidence-based interventions for all older adults in their care. These practices are known as the 4Ms: What Matters, Medication, Mentation, and Mobility.
Asking What Matters
When she was intermittently able to communicate, the team engaged Carmen directly about what mattered to her to align their care with her goals and preferences. When she could not say as much, they spoke with her family members. The team learned that when she was a young woman, Carmen had wanted to be an artist, and more recently she enjoyed drawing and sketching. She loved listening to gospel music and looking at pictures of her family members. Her family also shared examples of what had (and had not) helped her in the past.
How do you ask someone what matters? “Everyone asks [the question] differently,” said Priscilla Yee, MD, Geriatrician at the CLC. Yee, a geriatrician, has worked at multiple Veterans Affairs (VA) locations to improve care for older adults and completed an advanced geriatrics fellowship with the Geriatrics Workforce Enhancement Program. “[One team member] might ask, ‘What makes you happy? What brings you joy? What things do you like to do?’” she said. Yee herself often asks, “What are some things you would like me to keep in mind with regards to your health and your health care? What will be most important to you settling into the CLC?”
Carmen had told both her care team and her family that structure and routine were important to her mental health, so they noted this in her care plan. Certified nursing assistants worked to be consistent in how they approached her for breakfast or to get changed. They also made sure the routine was really hers. “Often, we subject people to routines of the health care setting,” said Yee. “For example, we make [residents] start their day when breakfast is served” and not when they want to get up.
Carmen was not an early riser, so she would have breakfast in her pajamas and go back to bed. At lunchtime, she would get dressed and take part in the recreational therapist’s afternoon activities. By honoring Carmen’s preference for participation when she was most alert, winning card games became both fun and supportive of her mentation and mobility.
A Team Effort
The team uses a multidisciplinary approach to address what matters to patients. “The heart of geriatrics is interdisciplinary,” said Yee. She describes the approach as, “All hands on deck.” Each Monday, a team including a psychologist, chaplain, recreational therapist, geriatrician, nurse, and pharmacist meet for behavioral health rounds. On Wednesdays, a clinical team that includes a psychologist, geriatrician, pharmacist, psychiatrist, and nurses discuss mental health and related issues.
It had been difficult to use certain screening tools with Carmen. “Her emotions and extreme tearfulness made it difficult for her to complete a full cognitive assessment,” explained Yee. “She hadn’t been fully assessed for depression because it was hard for her to sit through [an evaluation].” Consequently, she had been diagnosed with dementia without a full screening. The team questioned this conclusion because when she was mentally and emotionally stable, Carmen was lucid and organized. She would come to medical visits with a notebook she used to track her health appointments and a checklist of what she wanted to discuss. She also recognized Yee at each encounter. The team suspected that Carmen might be experiencing delirium.
Identifying and treating delirium was an interdisciplinary effort. The recreational therapists had been the first team members to identify the need to assess Carmen for delirium when her speech changed during weekly card games. “Usually, she was smack talking with the other players,” Yee explained. But then Carmen’s demeanor changed. “What she was saying was coming out of left field,” Yee recalled. Since the team was familiar with her typical behavior, they could see changes and communicate about their concerns.
Leading from the Frontline
Many team members have contributed to CLC’s age-friendly success. For example, Jacquelyn Claude, MSPH, BSN, RN, Nurse Manager of CLC-B, worked with the full nursing team to put the 4Ms into action. They created a mobility schedule for residents to move three times each day. The certified nursing assistants, who get older adults out of bed, were central to this process.
Staff created individualized plans for each resident. For example, they would help one person out of bed on Fridays because they know he is happy to be up when his son is visiting. “The frontline staff make a difference every day, providing top-notch care for our beloved veterans,” said Claude.
Frontline staff have also been central to rolling out a new delirium screening process. For some screenings, the older adult must interact with the screener and complete tasks that include reciting the months of the year backward. This was not appropriate for people with severe dementia or those who are nonverbal. Another tool, the NuDESC (Nursing Delirium Screening Scale), uses an observational checklist. The staff voted to use this tool. When nurses get a positive result with the NuDESC, they alert providers like Yee for follow up.
Claude includes the 4Ms in the nursing care plan for each new resident. Recently, a new resident arrived who had dementia and delirium. He had not walked in weeks after being hospitalized. The team learned that this resident loved music and found that playing music helped his mood and behavior. They adjusted his medication and his delirium improved. After working with a physical therapist, he was able to stand and sit in a chair with assistance. This increase in his mobility in turn helped further reduce his delirium.
Making Changes
Carmen also benefited from the care team balancing her different needs, including her mobility and her mentation. Medication played a key role here.
Carmen had been taking antipsychotics for many years, which caused drug-induced parkinsonism. “We didn’t want to put her on medication for the tremors since we knew they were caused by medication,” said Yee. Some medications could also increase her fall risk. Instead, the team got weighted utensils so Carmen could eat independently, partnering with the dietary team to add them to her meal trays.
To better treat her depression and help with delusions that were interfering with sleep, Yee increased the dose of some of Carmen’s medications. Once she was more stable, the team reassessed Carmen’s dosages and continued to monitor her closely for side effects.
Explore ways to get involved and join the Age-Friendly Health Systems movement
These days, when team members discuss Carmen’s care during rounds, they talk about how well she is doing. She is back to using a walker, as she did before her hospital stay. She is sleeping better, and her mood and overall mentation have improved. They know to pay attention to changes. For example, her family noted that Carmen sometimes finds the holiday season overwhelming, so as November and December approached, the team was on high alert and ready to respond.
Editor’s note: Since the events detailed in this post, Jacquelyn Claude has moved to the role of RN Nurse Navigator on the Referral Coordination Team.
Cayla Saret, MPH, is a Senior Managing Editor at the Institute for Healthcare Improvement.
Photo by bernie_photo
You may also be interested in:
How to Have Conversations with Older Adults About “What Matters”: A Guide for Getting Started A short guide for anyone who cares for older adults, in any setting, to help jumpstart conversations about What Matters most.
The Basics We (and Policymakers) Should Know about Nursing Homes
Centering What Matters: The Core of Age-Friendly Care
Caring for the Caregivers is Part of Optimal Age-Friendly Care
