Why It Matters
Photo by Claudio Schwarz | Unsplash
It may be clear to many people working in health care that lack of food security has a negative impact on patient health, but that understanding does not make the problem easy to address. For example, screening for any social determinant can seem invasive, especially without a clear way to address a need once it is identified. Also, without proper training, physicians and staff can feel uncomfortable asking questions about food stability and other issues.
How can health systems better screen for social determinants like food insecurity? How can we provide proper and timely assistance to patients, including meeting an identified need before a patient leaves an office visit?
These are some of the questions asked by Megan Cahn, PhD, MPH, Associate Scientist, Population Health at Legacy Health based in Portland, Oregon. Legacy was one of three health systems that participated in a year-long learning and action network (LAN), facilitated by the Institute for Healthcare Improvement and sponsored by Pfizer, to support organizations seeking to integrate social health into care delivery in pursuit of improved health, well-being, and equity for their populations. Three integrated delivery networks in the US were chosen to participate through a competitive grant award process.
Legacy chose to focus their work on food insecurity based on how the issue was affecting their community. Legacy found that food insecurity was the most prevalent social need identified by patients, including 41 percent of Medicaid members and 23 percent of Medicare members. Food insecurity is also associated with negative health outcomes, particularly diabetes and hypertension. Patients experiencing food insecurity and diabetes have higher health care utilization rates across outpatient settings and higher health care costs compared to patients without diabetes. Food insecurity is also associated with cost-related non-adherence to diabetes management, which leads to poorer health outcomes. One of the ways Legacy was able to garner support for expanding their program was underlining how tackling food insecurity could both improve outcomes and reduce costs for patients in the highest level of health care expenditure.
Legacy began with the aim of improving access to food from their medical center, but when they realized that their clinics needed better screening support, they quickly pivoted to focusing on screening and developing their program of direct access to food. Initially, staff were not comfortable offering food resources without a standardized, non-biased way to ask patients about food security. Over the course of the year-long LAN, the Legacy team worked on improving social determinants of health screening and referral; establishing sustainable food security programming for food insecure patients and families; improving physicians’ ability to understand, assess for, and integrate social determinants of health in routine patient care; and expanding collaborations with community partners and organizations.
Legacy has made incredible progress. This year, they have provided over 1,800 bags of food to their patients and have secured funding to continue the food bag program. By the end of the LAN, all 25 of Legacy’s primary care clinics had started screening for food insecurity, up from 11 when the LAN began. Figure 1 below illustrates the progress Legacy has made in their screening rates, particularly among the new adopter clinics.
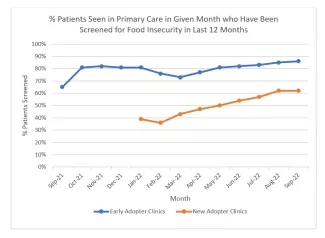
Figure 1. Legacy Health primary care food insecurity screening data
Legacy has also secured additional staffing to better support the food bag program. Their additional team members will provide budget management support, provide access to food insecure staff, and serve as community health workers.
Going forward, some of Legacy's ongoing work will be to make the contents of their food bags more nutritious for patients, especially those with diabetes. Currently, most bags include items like pasta and sauce, peanut butter and jelly, fruit cups, and soup. While three of Legacy's sites offer fresh food — including fruits and vegetables, eggs, yogurt, and bread — their overall efforts are often limited to shelf-stable options and by supply chain constraints.
Keys to Success
- Partner with staff. The keys to expanding screenings were spreading awareness about food insecurity and providing education on how to properly screen patients. The team met regularly with clinic staff involved in the process (including medical assistants, clinic managers, nurse case managers, social workers, and patient navigators) to discuss the importance of the screening and to learn how to best implement this work. Based on those discussions, they developed a screening workflow and FAQ sheet. Education about screening was also incorporated into an annual training on the social determinants of health for Legacy's internal medicine residents.
- Integrate changes into existing workflow. For Legacy, this allowed easier uptake for clinic staff, leading to higher screening rates. Specifically, they added the food insecurity screener to the existing pre-visit summary documents that patients complete when they arrive for appointments. These questions are also in the electronic health record Legacy uses and this allows for easy data entry and reporting.
- Work with community partners. A major project the Legacy team undertook was implementing a pilot program with an online platform that connects patients to resources in their local community. The goal of the referral pilot was to provide improved social service referrals and closed loop referral data. Connecting all the partners to the referral platform has been a source of some challenges, but connections to community partners have been instrumental to getting patients the resources they need.
- Engage leadership. Tackling social determinants can be considered outside the traditional scope of health care operations. But Legacy Health leaders have made it clear that they see addressing these needs as essential to fulfilling the organization’s mission to help everyone in their community live healthier and better lives. As a senior leader at Legacy told the LAN team, “The way to move this work forward in the health system is to not ask if, but ask how.”
The team is encouraged by the progress they see. According to Cahn, a lead medical assistant shared that it used to be difficult to get staff to hand out food bags before screening started. “With the screening in place, it feels less invasive to be discussing food insecurity with patients,” the medical assistant said. “Now, everyone seems excited about the program.”
You may also be interested in:
Addressing Loneliness to Promote Health
Understanding the Social Determinants of Health and What Gets Missed When You Don't
