Why It Matters
While the future of telemedicine beyond the pandemic is unclear, it is highly likely that its use will continue to evolve, and the six essential elements of safe, equitable, and person-centered telemedicine — access, privacy, diagnostic accuracy, communication, psychological and emotional safety, and human factors and system design — will require continued attention. The following is an excerpt from the Telemedicine: Ensuring Safe, Equitable, Person-Centered Virtual Care white paper focused on human factors and system design.
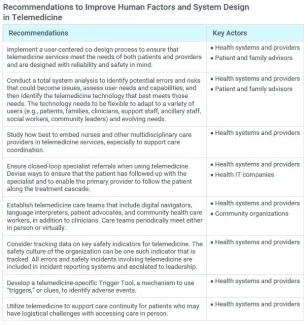
It is essential for telemedicine services to be fully integrated into the existing system, not just added on — and this might require fundamentally reimagining the entire system. The design of telemedicine services must ensure that the system is reliable, safe, efficient, and person-centered. The IHI white paper, A Framework for Safe, Reliable, and Effective Care, presents two components that provide the foundation for creating systems of safety: culture and the learning system. Foundational principles that make systems and processes more reliable include standardization, simplification, reduction of autonomy when standardized processes exists, and highlighting deviations from standard practice.
Human factors are also an important consideration for system design, that is, “the interaction of human abilities, expectations, and limitations, with work environments and system design.” The most foundational human factors consideration is that the patient needs to be prepared to use telemedicine technology and the methods involved in virtual care. Providers must also be comfortable with and adept at utilizing telemedicine technology. Innovation may be required to ensure both access to and the ability to use the required technology.
Another important human factors element is responsiveness to important cues that might be missed when care is provided virtually. Missed cues may lead to diagnostic errors and decrease trust between provider and patient.
Telemedicine also requires providers to learn new or adapted approaches to manage data and health systems must ensure that the technology is integrated and interoperable with the existing IT infrastructure. Telemedicine services must be designed to ensure coordination and continuity of care.
Through user-centered co-design, active learning, and feedback loops, organizations need to continuously monitor, assess, and adapt every aspect of telemedicine as needed. This process may include collaboration within the organizational learning system and with community partners, particularly when community resources are included in the design of telemedicine services. In addition, health care delivery systems need opportunities to participate in open forums to share lessons learned and best practices among organizations. As telemedicine design and implementation takes shape, assess whether the desired outcomes are being met and mitigate potential risks as they are identified.
Human factors and system design are elements of the framework for ensuring safe, equitable, person-centered telemedicine. To learn more, download the free Telemedicine: Ensuring Safe, Equitable, Person-Centered Virtual Care white paper.
You may also be interested in:
Telemedicine Can't Get Safer Without Bridging the “Digital Divide”
